Review of Treatment Goals
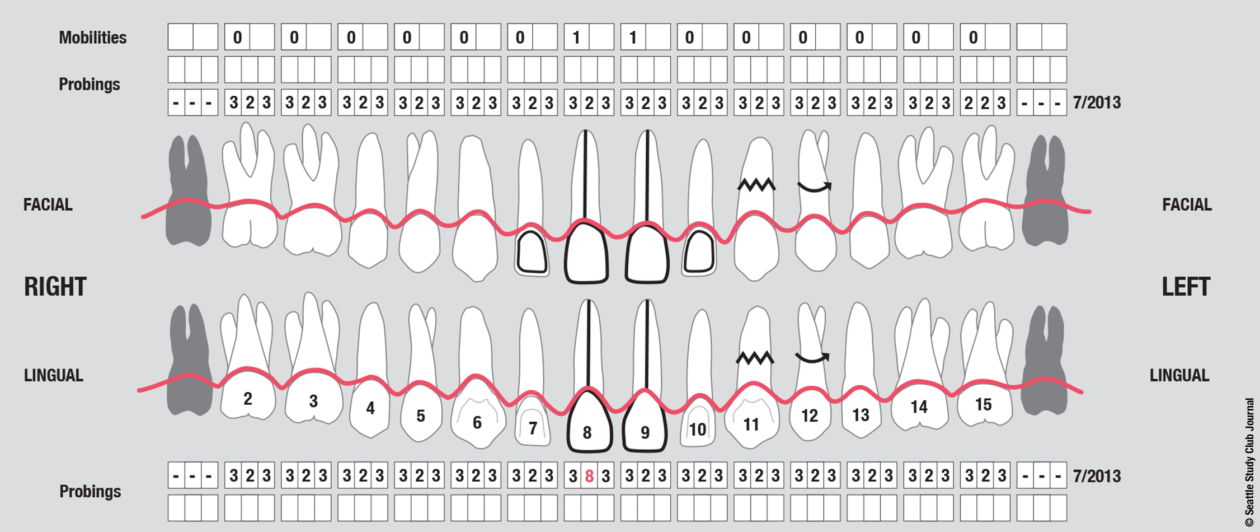
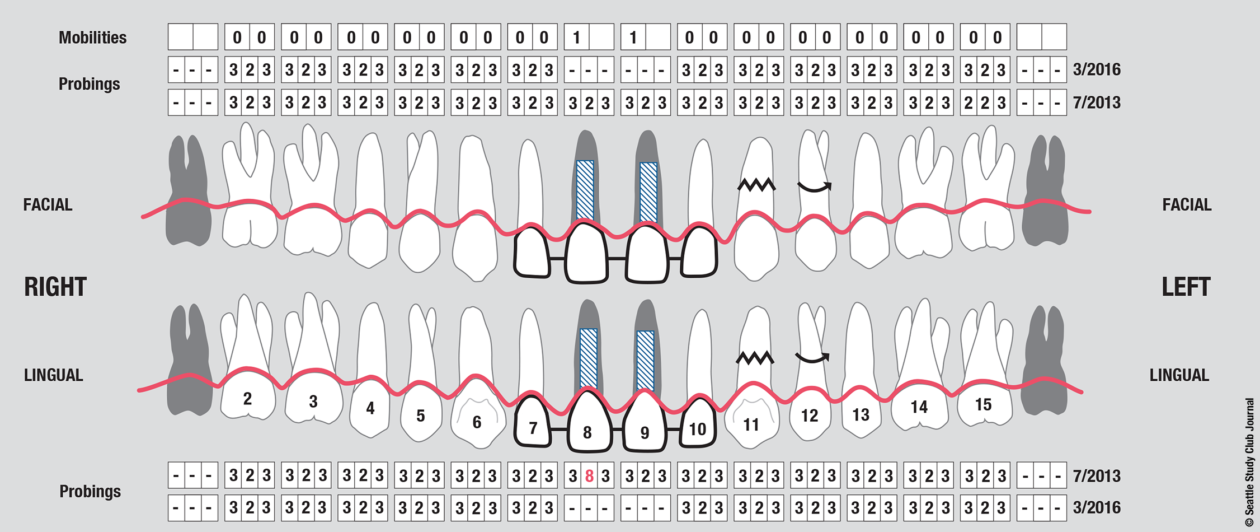
The patient presented with an initial concern about the appearance of her smile and a fistula at tooth no 8. She completed orthodontic therapy in 7th grade but was elbowed in the mouth a few years later and sustained an injury that went untreated for 2 years and ultimately required root canal therapy on teeth nos. 8 and 9, followed by a tissue graft. At age 20 she had veneers placed on those teeth. Four years later she had root exposures, and new veneers were placed on teeth nos. 7–10. In 2011, the veneers on teeth nos. 8 and 9 were replaced with crowns. In 2012, she awakened one day in an open locked condition.
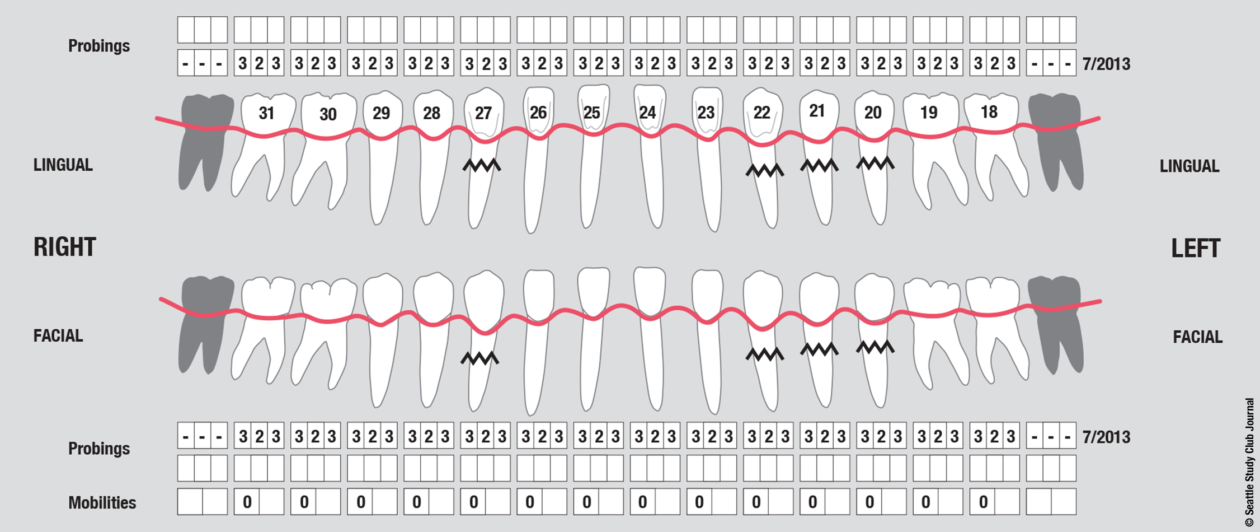
The immediate goal of treatment was to deal with the failing and infected teeth nos. 8 and 9. Once that situation was stabilized, the functional goal was to provide a long-term solution for the replacement of missing teeth nos. 8 and 9 and correct the malocclusion. The patient’s esthetic goals were to make the anterior teeth wider and longer, create a wider smile, correct the malpositioned tooth no. 27, and replace the unesthetic Class V restorations.
Phase I: Tooth Extraction and Provisionalization
Teeth nos. 8 and 9 were extracted, the sockets were preserved with rhBMP-2 and cancellous allograft, and a provisional from teeth nos. 7 to 10—with nos. 8 and 9 functioning as ovate pontics—was delivered.
Phase II: Surgery
Surgically facilitated orthodontic therapy (SFOT) was initiated with corticotomies and decortication of the maxilla and mandible with the goal of expanding the arch forms and optimizing the transverse, A-P, and maxillomandibular relationships. SFOT was performed using mineralized freeze-dried bone allograft (FDBA) and Bio-Oss (Geistlich) combined with platelet-rich fibrin. Interpositional connective tissue grafting comprising autogenous tissue and Emdogain (Straumann) was undertaken for mucogingival augmentation in the areas of teeth nos. 21, 22, and 27. Horizontal and vertical tissue engineering via rhBMP-2 and cancellous allograft was completed at the sites of teeth nos. 8 and 9 for edentulous ridge augmentation.
Phase III: Implant Placement
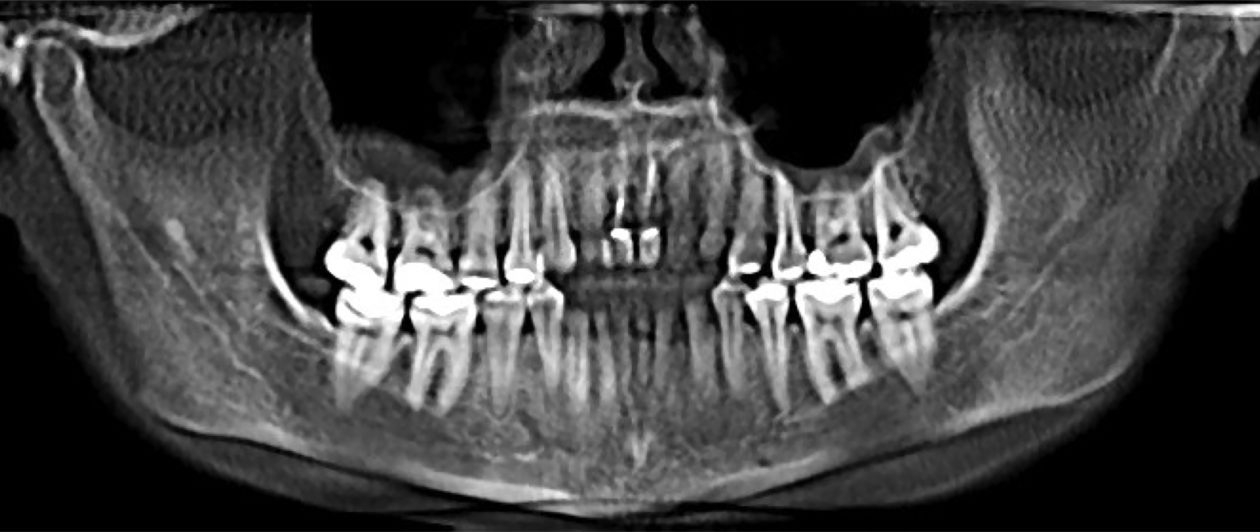
Eight months after completion of the SFOT, implants were placed (guided) at the nos. 8 and 9 sites via CBCT static guides. Contour bone grafting was performed using small-particle xenograft (Bio-Oss) + barrier membrane (Bio-Gide, Geistlich) for optimal peri-implant bone volume in combination with autogenous connective tissue for soft tissue volume. Hard and soft tissue grafting at the time of implant placement was performed to optimize the pink esthetic volume and position.
Phase IV: Placement of Healing Abutments
Four months later, temporary healing abutments were placed as “tent poles” on the nos. 8 and 9 implants and covered with an additional connective tissue graft.
Phase V: Implant Uncovering
Three months later, the nos. 8 and 9 implants were uncovered, and aberrant frenum tissue was removed.
Phase VI: Implant Provisionalization (2015)
Following healing from implant uncovery, the provisionalization phase of the case ensued. This required several appointments for seating provisionals and working with contours to groom the soft tissues. The goal was to complete the case with conventional prosthetics, but despite all efforts the final bone topography did not support ideal tissue positions.