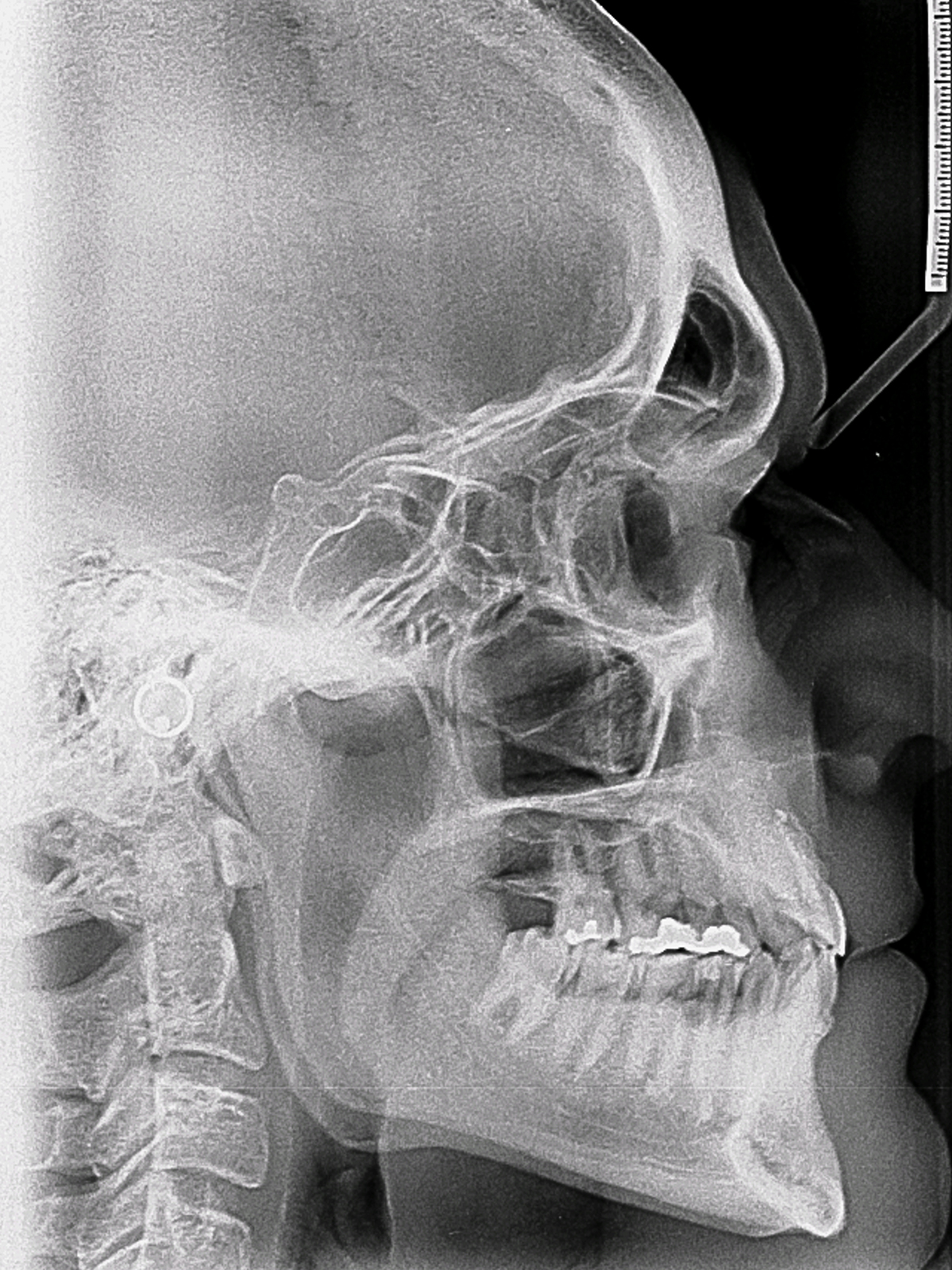
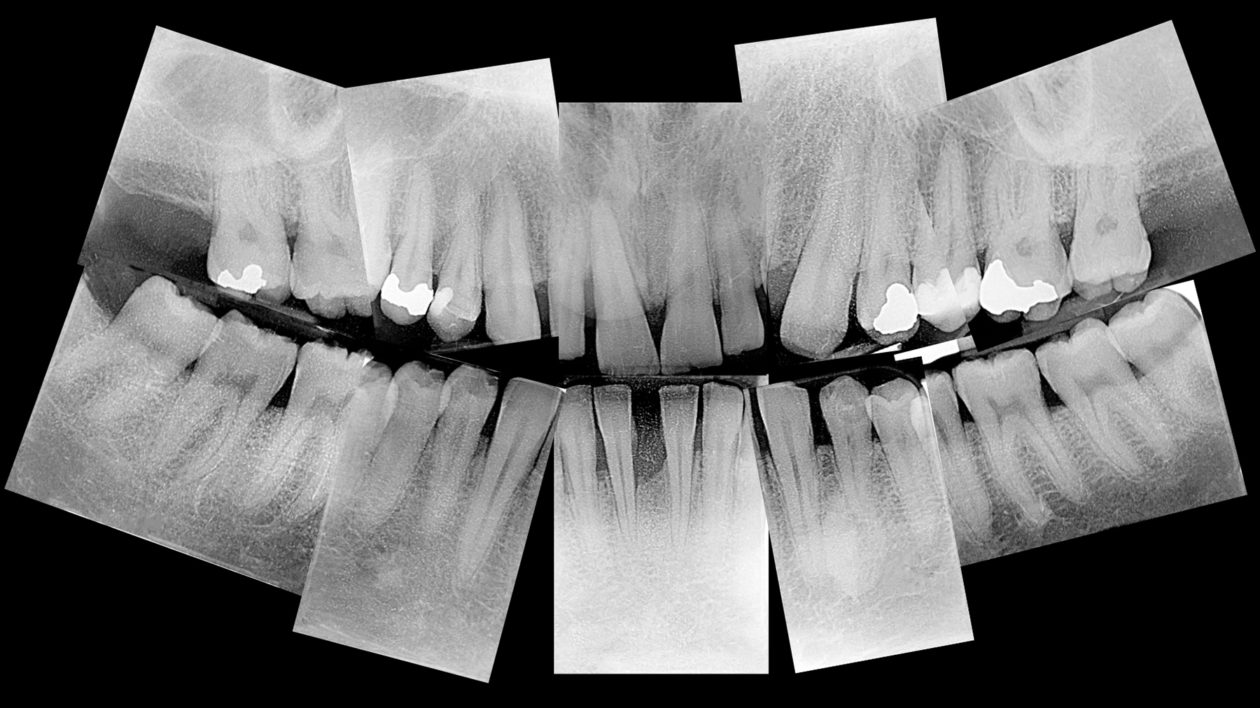
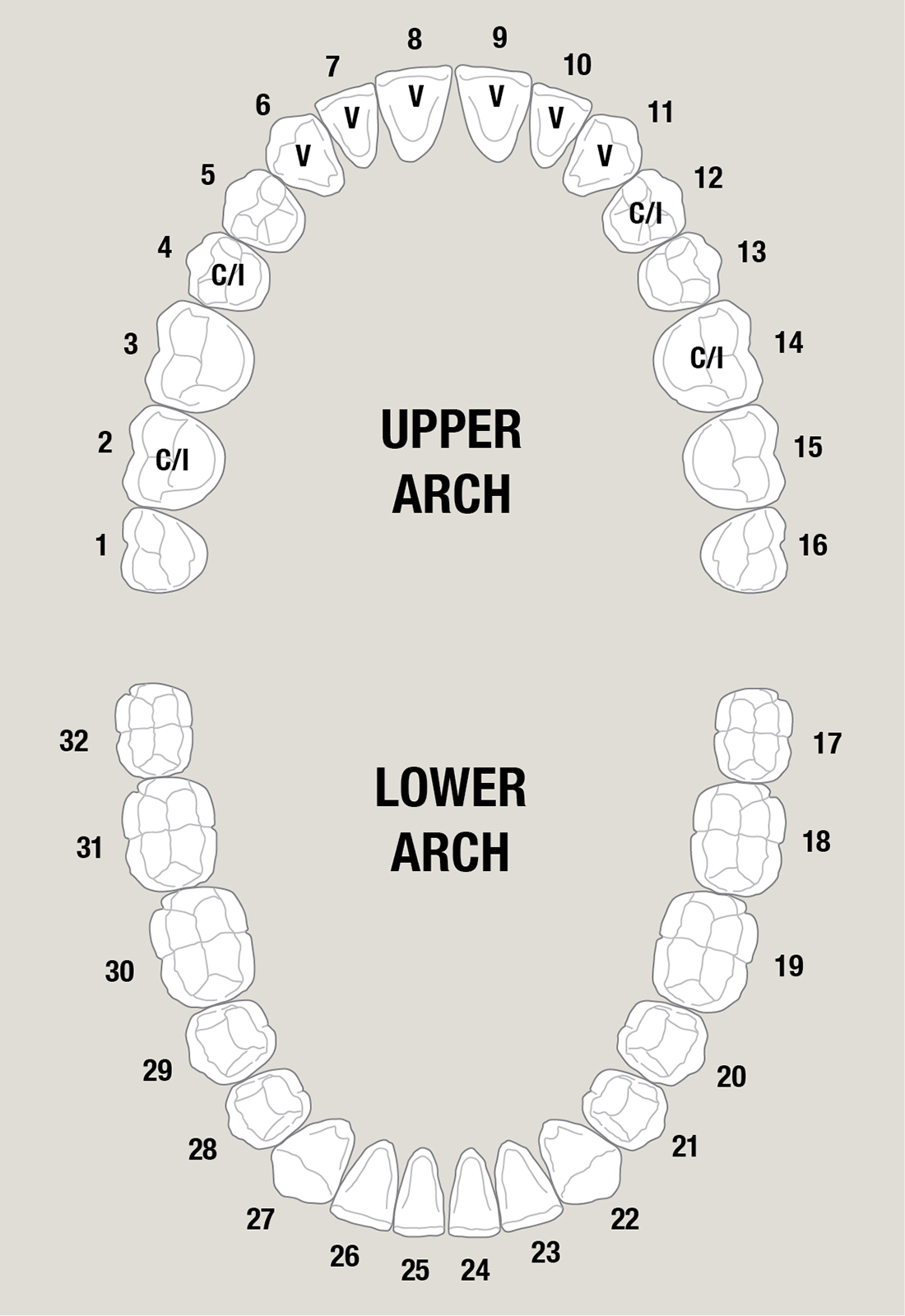
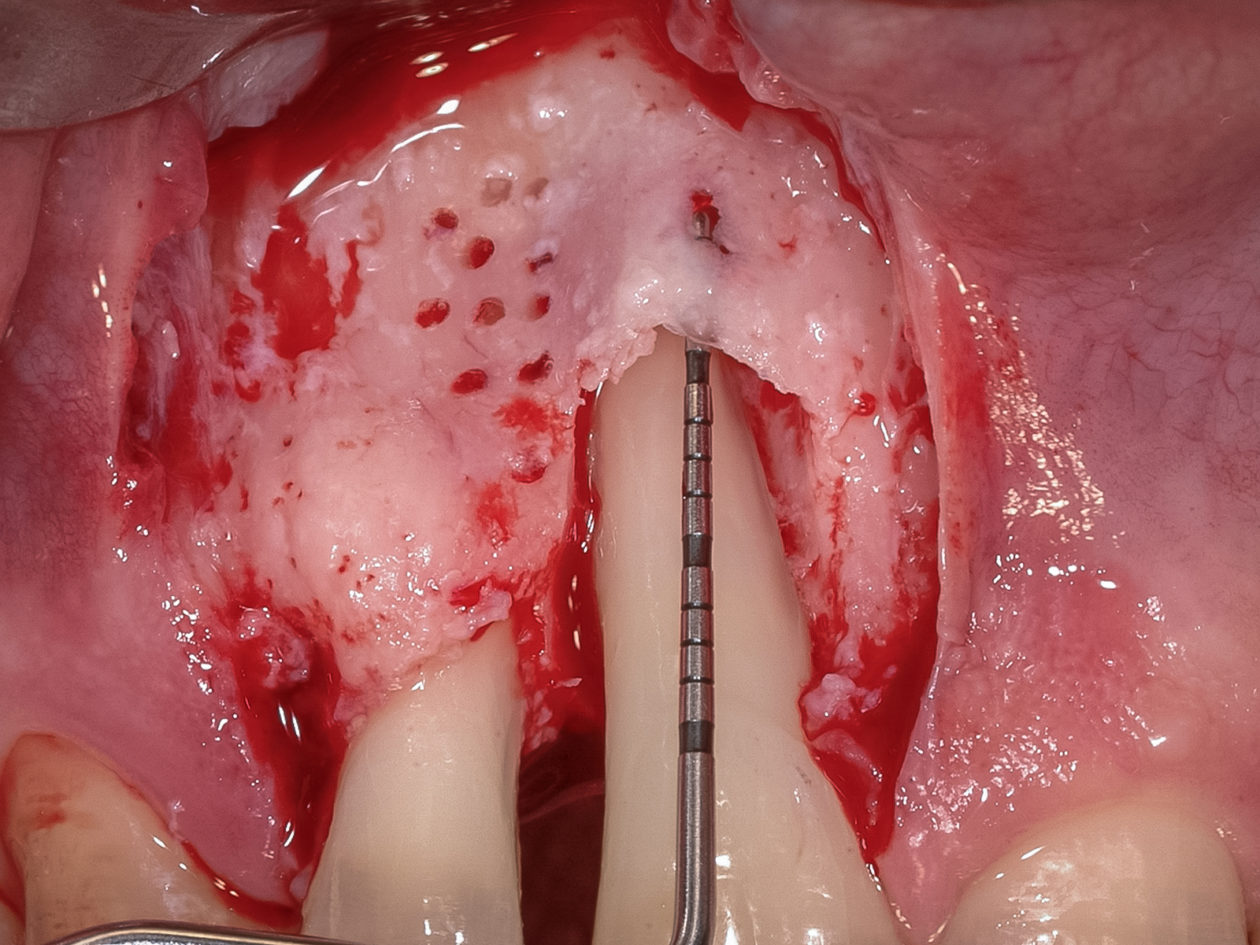
Case 102: In a World Where Implant Dentistry Dominates, Sometimes Traditional Periodontal Treatment Is Still Best
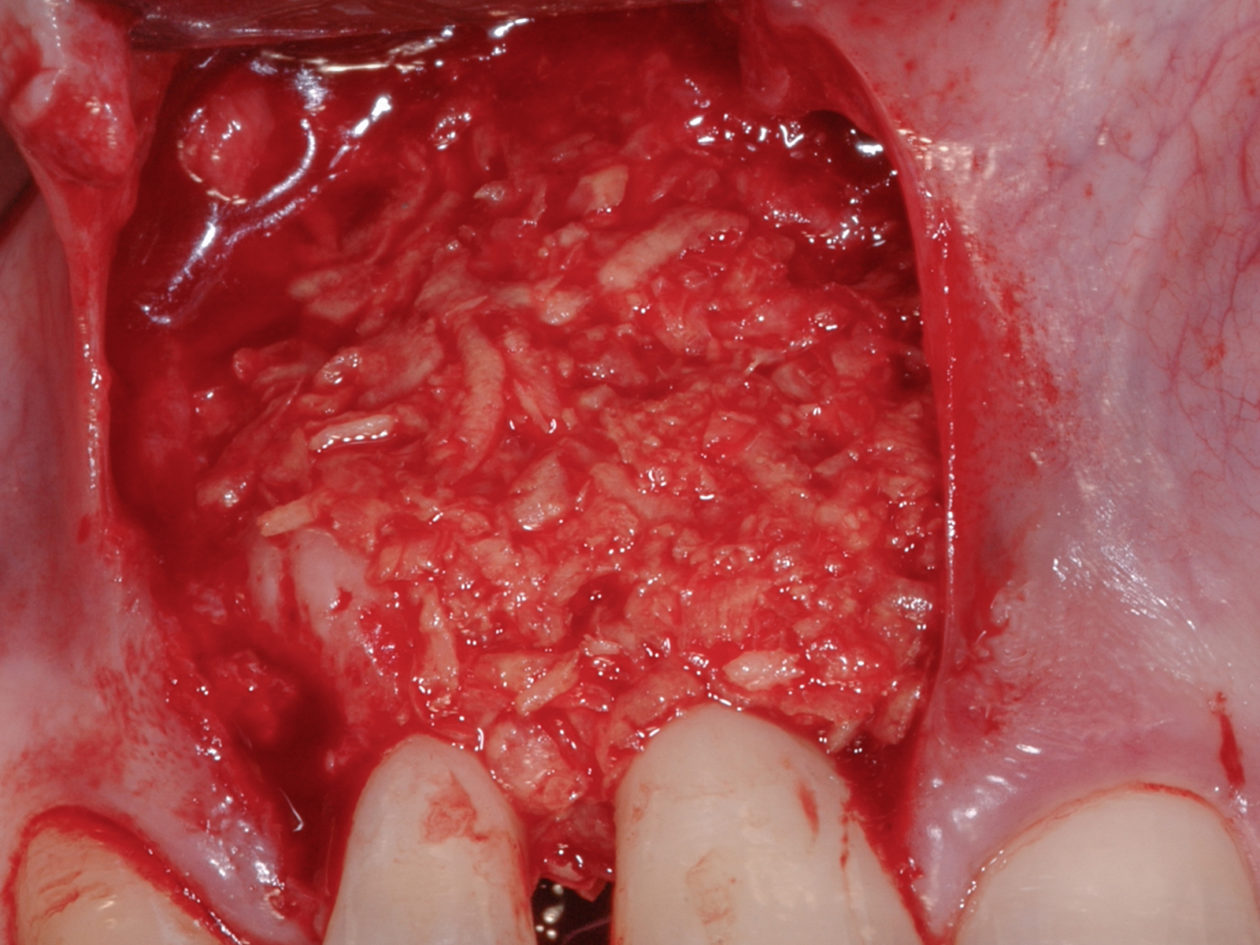
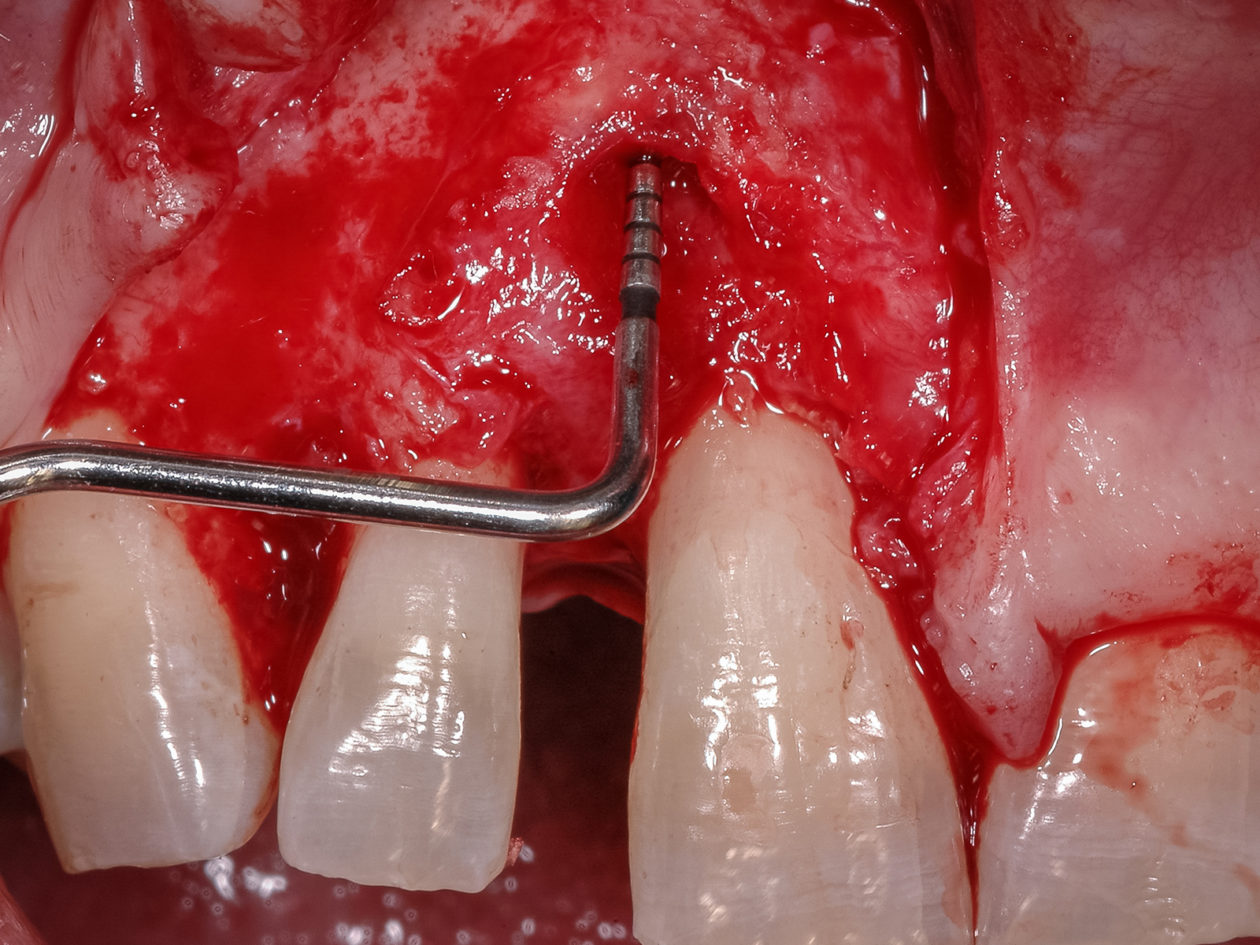
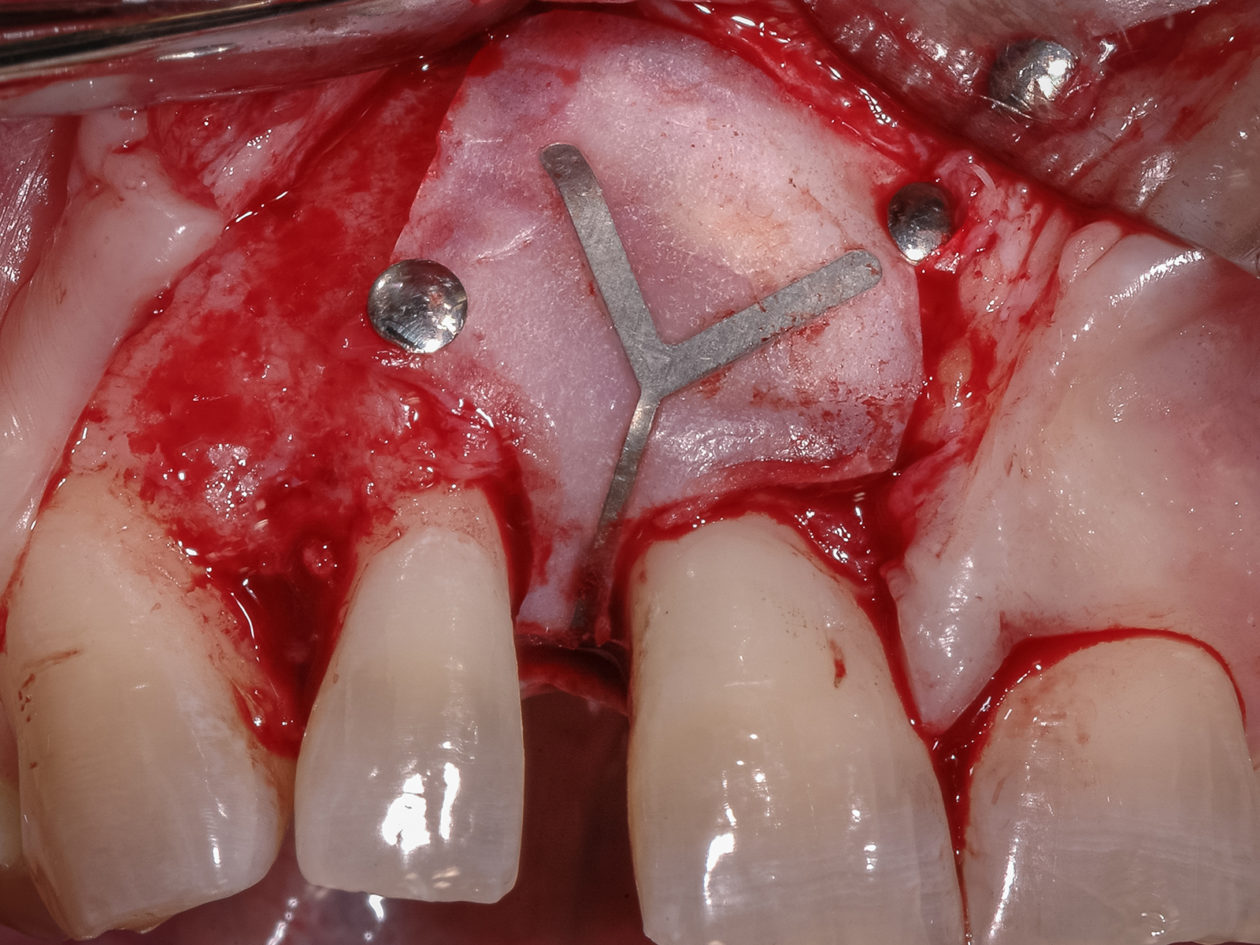
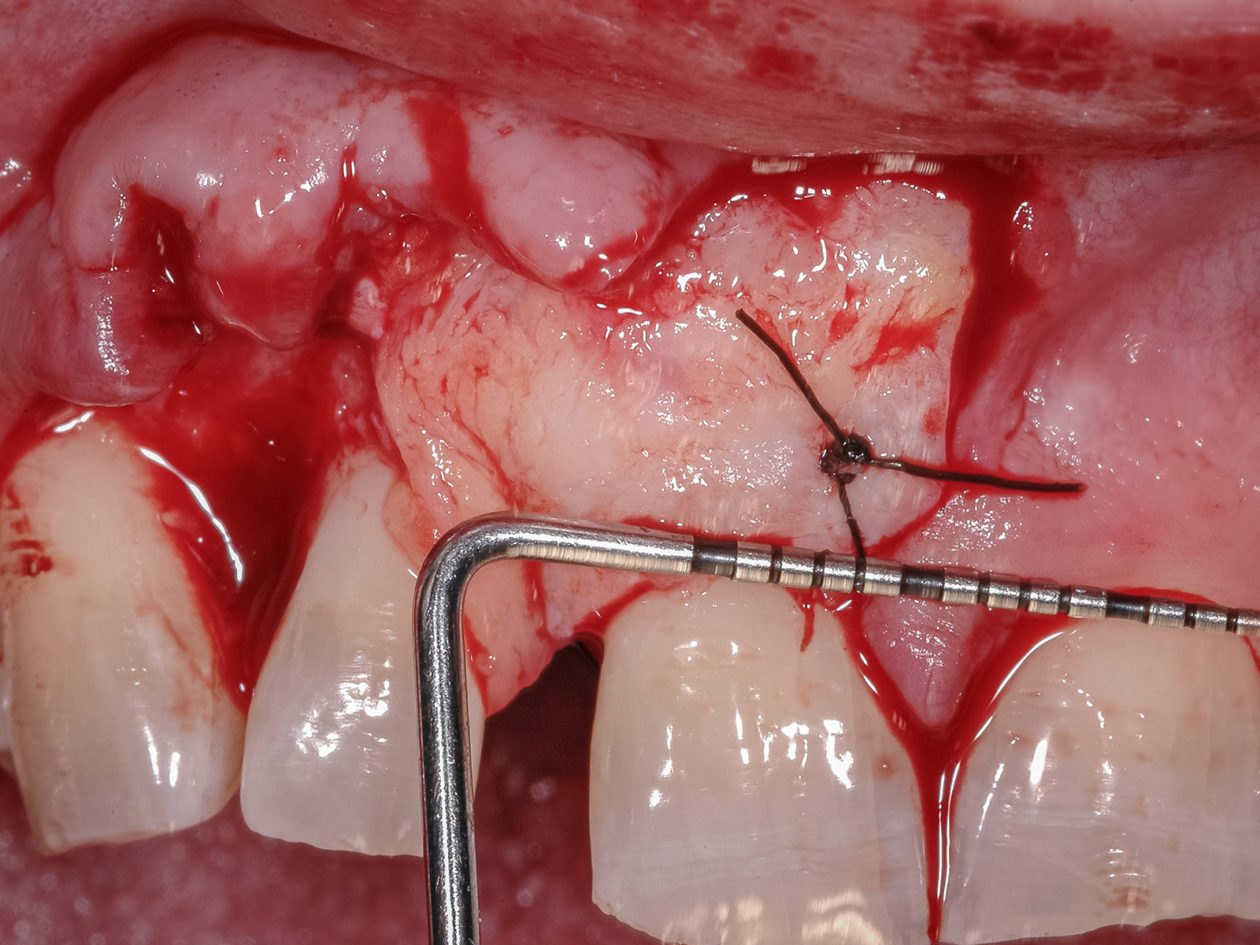
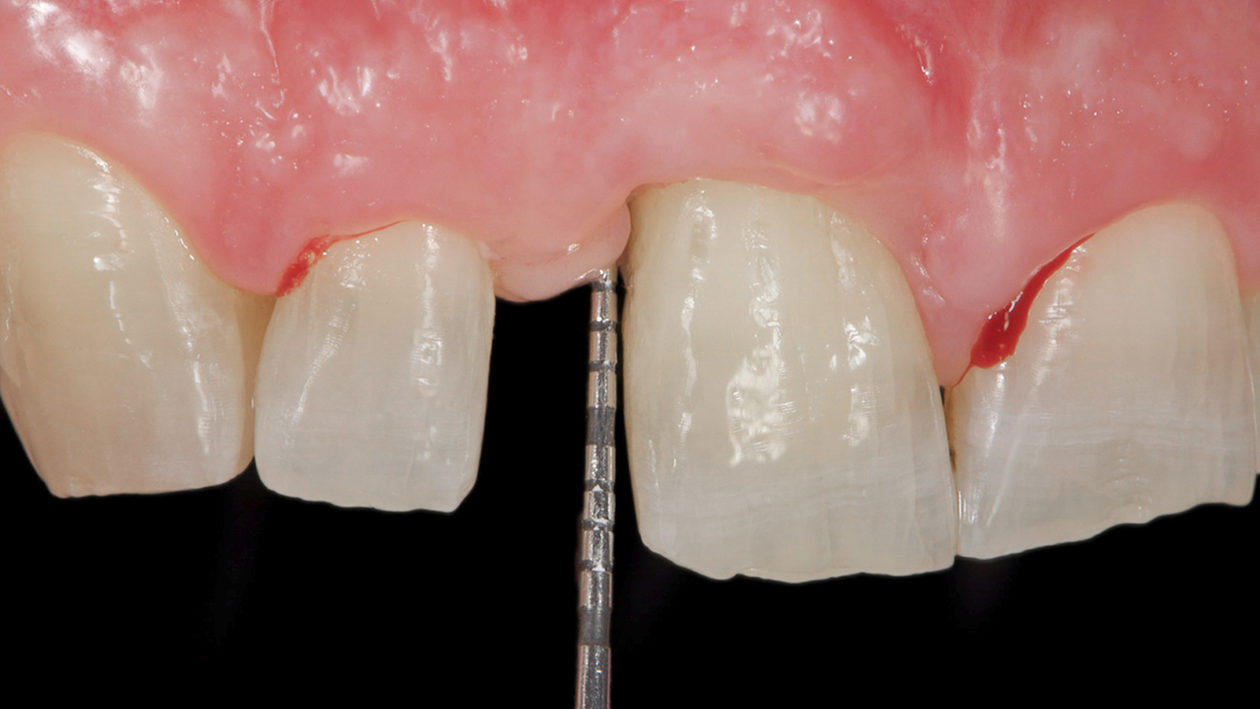
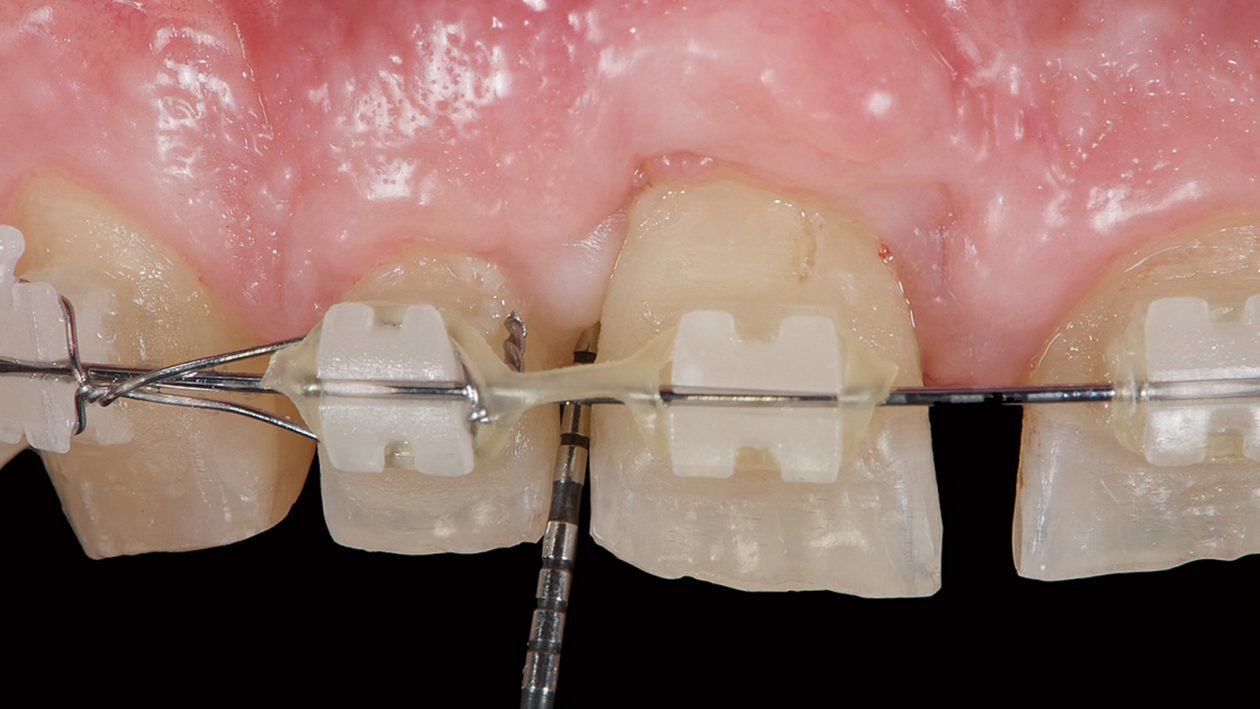
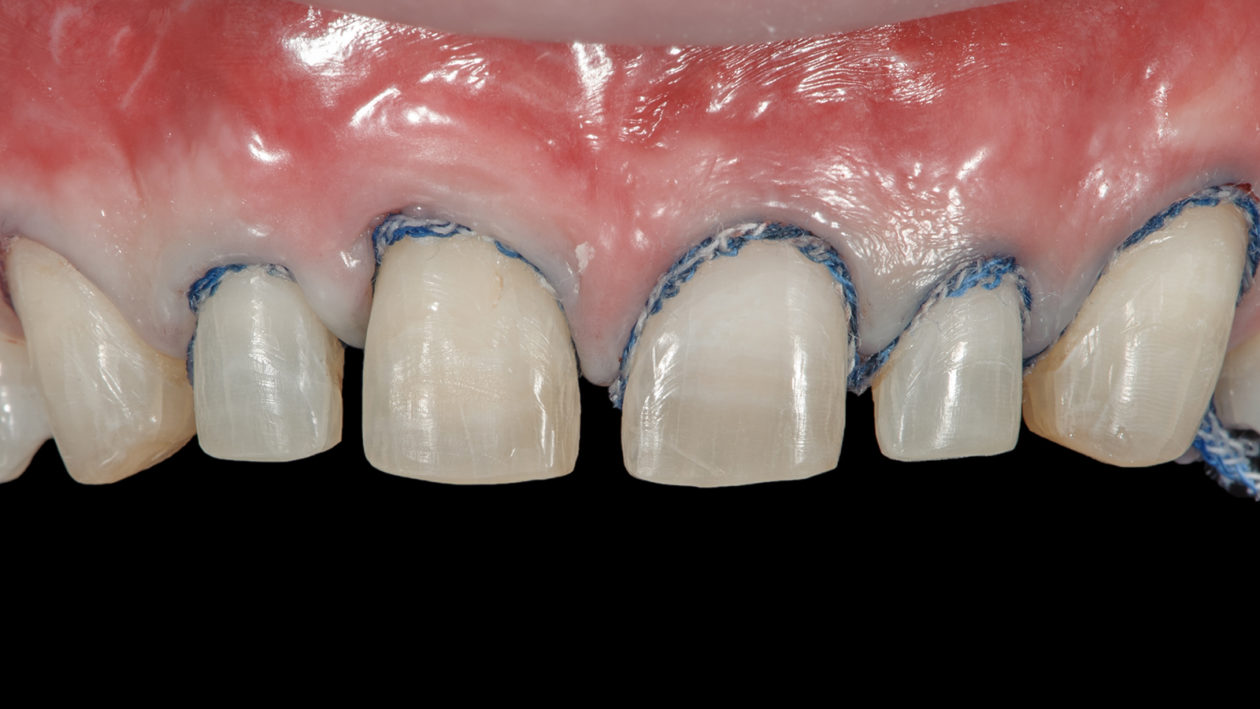
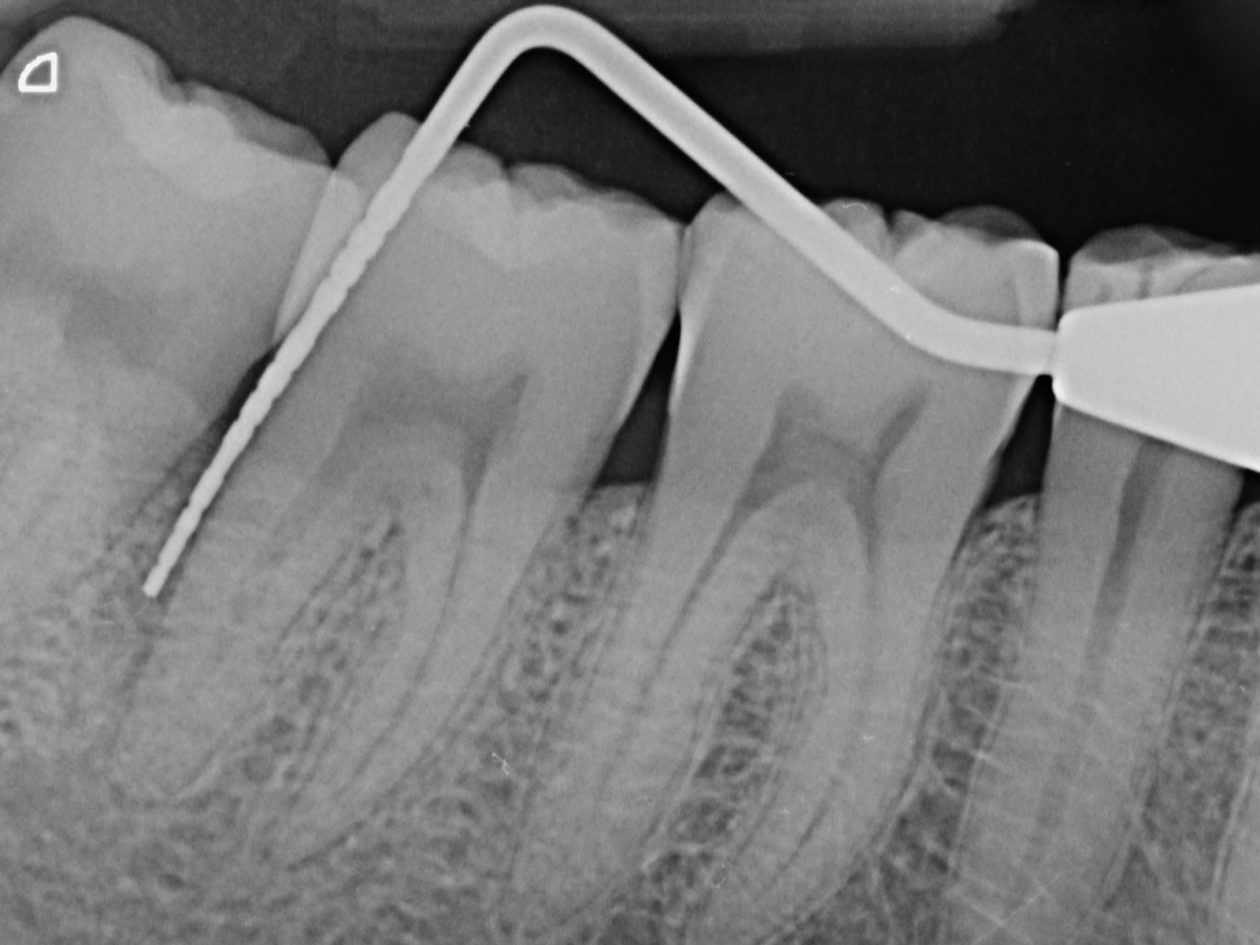
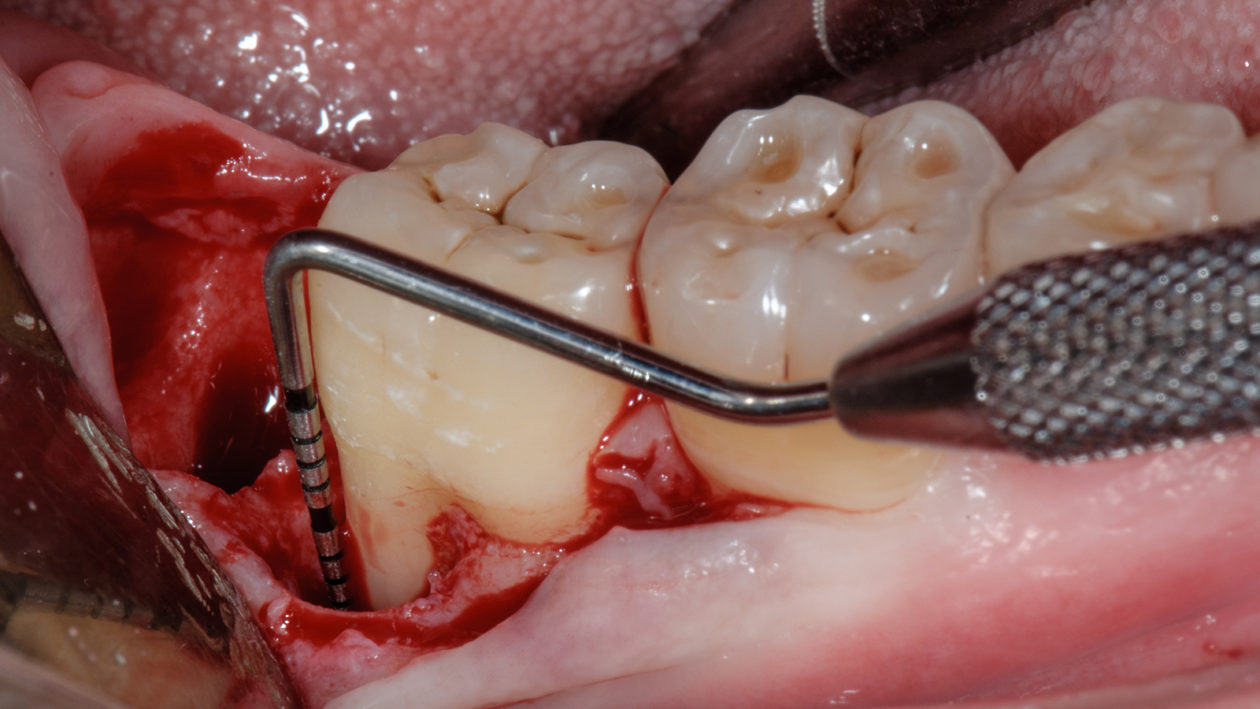
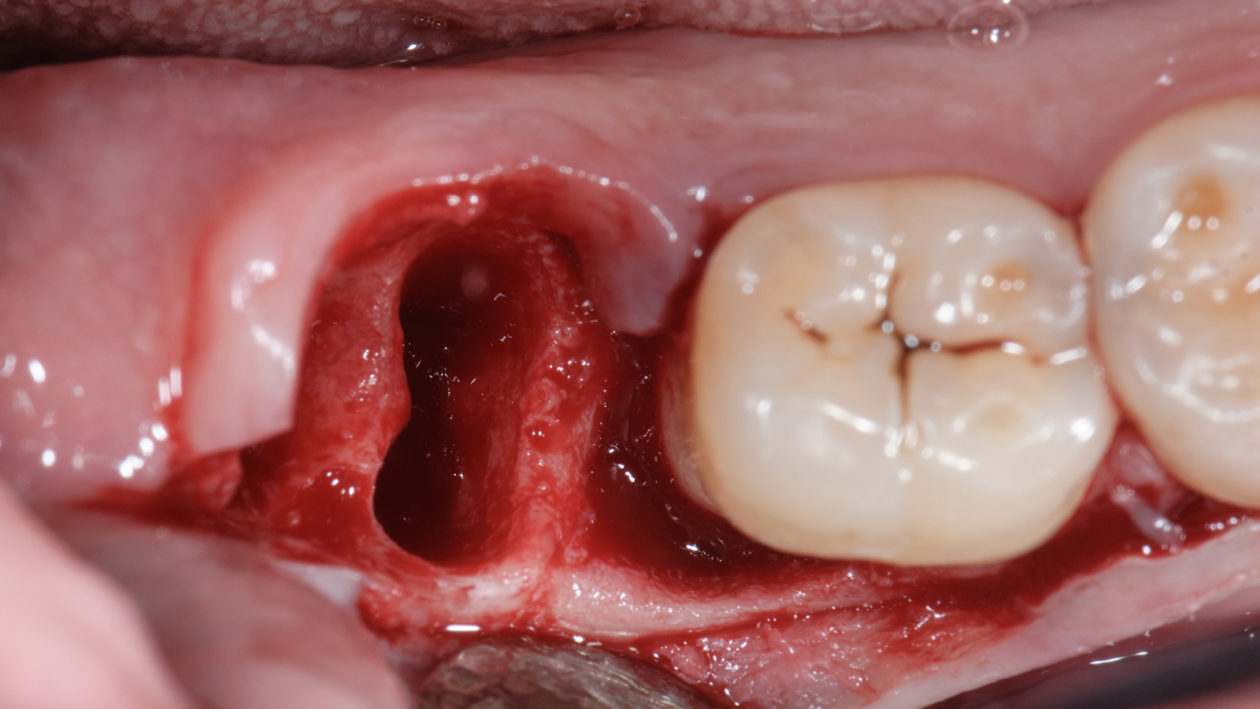
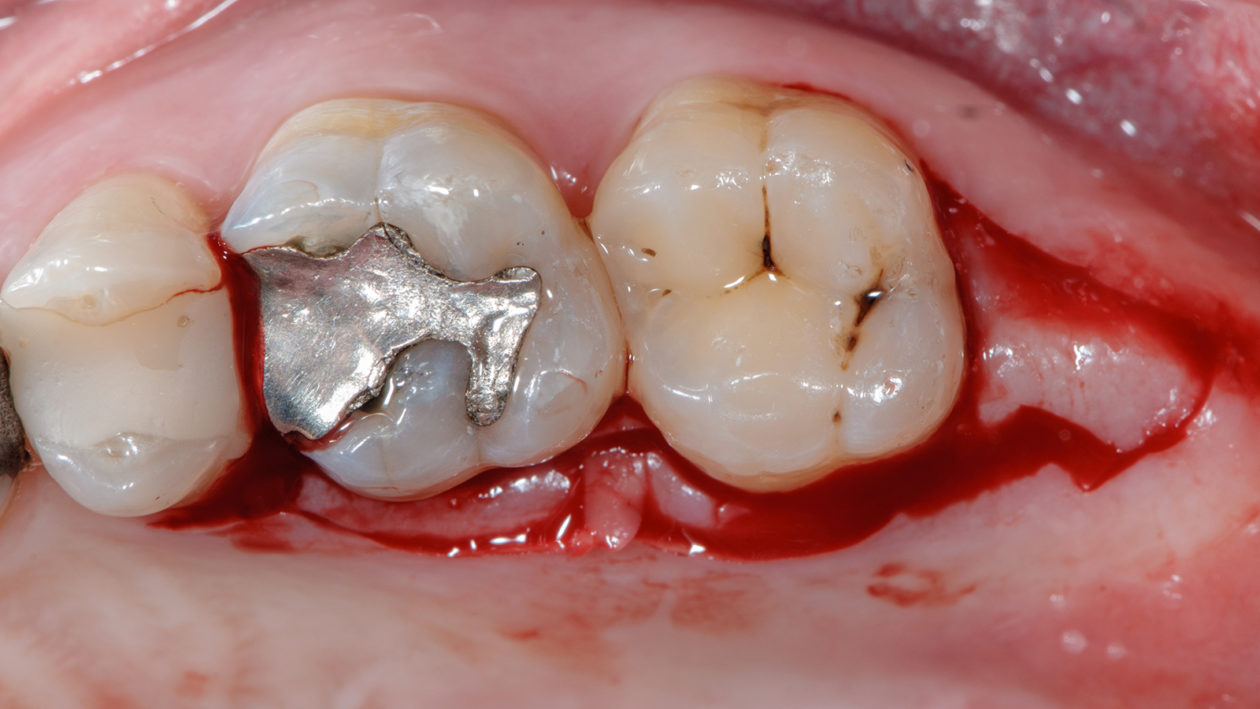
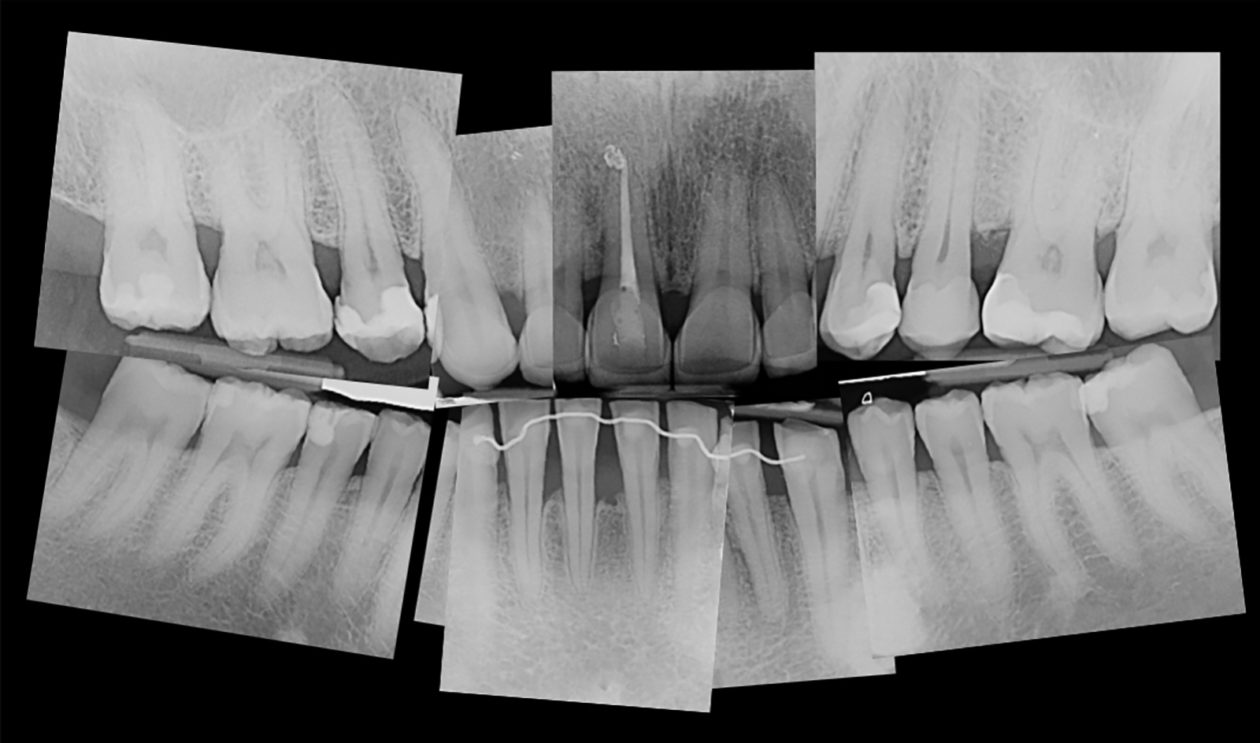
The patient presented with the chief complaint of pain and suppuration on tooth no. 8. He expressed that he had been previously treated for periodontal disease and had undergone bone regeneration surgery. He reported having regular brushing habits and consistent use of dental floss, interproximal brushes, and oral rinses.